Thank you for attending re:MARS
When the on-call surgeon gets word she’s needed in the operating room, she immediately opens the case on her tablet. A specialized algorithm has already aggregated the patient’s medical history from multiple providers as well as uploaded the latest images and scans of his abdominal injuries caused by a vehicle collision.
Each visualization provides critical information about the most appropriate interventions by drawing on the collective experience of the finest trauma surgeons from across the globe. One aspect of a perforated bowel repair looks particularly tricky—she reviews several of the recommendations to see which approach makes the most sense before sitting down at a control center, placing her hands on two ergonomic joysticks, and instructing a multi-armed surgical robot to make an incision.
Remarkably, the surgeon does all this while physically seated more than 500 miles away from the patient. She will rely on the robot, provided with autonomous capabilities through advances in artificial intelligence algorithms, to provide this life-saving surgical care. This is just one of many potential use cases for autonomous surgical robots.
“As surgeons, so much of what we do for patients has some collateral damage attached to it,” said John R. Adler, M.D., a neurosurgeon at Stanford University and founder and CEO at ZAP Surgical Systems, a company that specializes in gyroscopic radiosurgery systems. “We need better ways of doing surgery—and AI is an important part of the story of how we can get there.”
A new form of mythology
Over the past two decades, the use of surgical robots has grown dramatically. For example, Intuitive’s Da Vinci Surgical System allows surgeons to perform laparoscopic procedures with a greater degree of precision and control than they could with an old-fashioned scalpel and clamps—resulting in smaller incisions, less bleeding, and faster recovery for patients.
 Medical team supervises the Da Vinci robot-assisted procedure on screen. Photo source: Intuitive Surgical, Inc.
Medical team supervises the Da Vinci robot-assisted procedure on screen. Photo source: Intuitive Surgical, Inc.
Today, the world’s leading medical centers routinely use surgical robots in neurosurgeries, endoscopies, biopsies, arthroplasties, and other types of surgical procedures with differing degrees of human supervision.
Sandip Panesar, M.D., a physician, data scientist, and research fellow at Stanford University, said that futurists have been discussing the potential of autonomous surgical robots since the Smart Tissue Anastomosis Robot (STAR), guided by AI-control algorithms, showed it could suture reattach a resected intestine in a live pig both faster and more accurately than experienced surgeons.
However, Panesar strikes a cautionary note.
“There are different robotics companies that are heavily investing in AI to augment surgery,” he says. “But we are years away from any sort of fully autonomous system in clinical practice, even for more mundane surgical tasks.”
Axel Krieger, Ph.D., head of the Intelligent Medical Robotic Systems and Equipment (IMERSE) Lab at the Johns Hopkins University and the creator of STAR, agrees.
“Where AI can be of great use today is with image analysis,” he explained. “A big problem in surgery is the ability to recognize different structures in the body. If you think about what you see when you open up the body for surgery, it’s just a sea of pink. By analyzing large data sets of images, AI can help surgeons detect tumors or find the bladder neck you are trying to find. It can help differentiate healthy from diseased tissue, or point out that artery that you definitely don’t want to cut. That’s where we are already seeing the use of robots—and where current robots could deliver immediate improvements.”
Ken Goldberg, the William S. Floyd Jr. Distinguished Chair in Engineering at University of California, Berkeley, whose laboratory is currently working on an autonomous surgical suturing system, says that the surgical robots used today are much like AI-driven features in high-end automobiles. They can enhance rather than replace surgeon’s abilities in the OR. They may have some autonomous capabilities—however, they still require some expert supervision, especially when you are talking about tasks as high stakes as surgery.
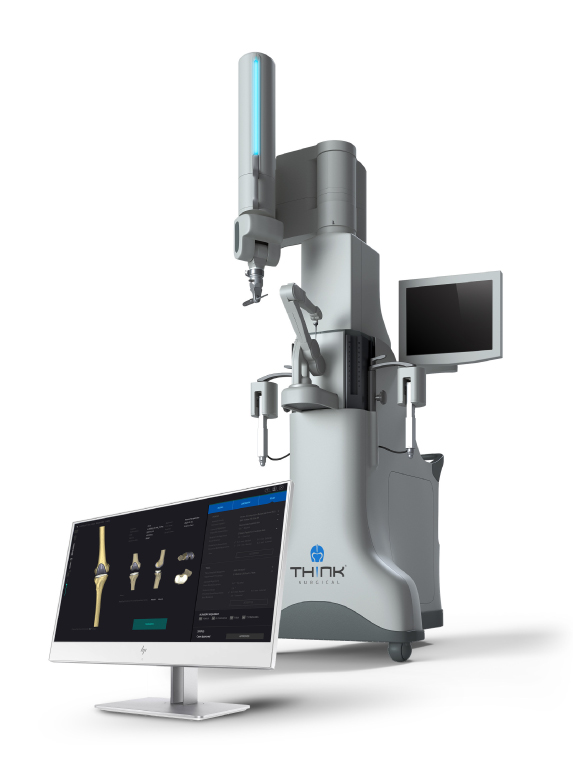 The TSolution One Total Knee Application is an active robot system for total knee replacement that supports an open implant library, giving surgeons a choice of implant options. Photo source: THINK Surgical, Inc.
The TSolution One Total Knee Application is an active robot system for total knee replacement that supports an open implant library, giving surgeons a choice of implant options. Photo source: THINK Surgical, Inc.
“What we’re really talking about is robot-assisted surgery—and that’s likely what we will be talking about for a long time,” he said. “Your car may have things like cruise control and anti-skid braking to support the human driver, and make driving safer, while at the same time, relieving the tedium of driving. These robots offer the same sort of capabilities. They can constructively assist the surgeon by performing some tedious surgical sub-tasks, so that surgeons can spend their time and energy on the more complex aspects of different procedures.”
Getting to an autonomous robot
“The research I do involves building robots completely from scratch,” says Pierre DuPont, Ph.D., Chief of Pediatric Cardiac Bioengineering at Boston Children’s Hospital. “A surgical robot has three basic components that you need to optimize. The first is the fundamental skeleton of the robot. On top of that, you can layer different sensing and control algorithms, integrated planning, and adaptation components to help you improve the performance of a particular task. The third component is what you think of as autonomy or AI. But to build a clear case for adding value, we have to overcome several challenges.”
The biggest challenge blocking widespread use of artificial intelligence in clinical settings is generalizability. Simply stated, a generalizable algorithm is one that works at the same level of accuracy across all circumstances, regardless of what images you use, what surgical workflows you employ, or what race, ethnicity, age, or sex of people you treat. To develop truly generalizable algorithms, AI developers need access to train robots on highly diverse clinical data to help them differentiate between colon and intestine, blood and bile, cancerous cells and healthy tissue.
“It’s very hard to see what’s going on inside the body, especially through a camera,” said Goldberg. “The surfaces are deformable. They are spectacularly shiny with blood and other liquids. There are often many obstructions because of other organs or blood. On top of that, every patient is different. No two bodies are built exactly the same way—so there’s very little uniformity to build upon to make generalizable algorithms.”
Panesar said that many of the AI solutions that have been successful work so well because they are limited to a specific part of the body.
“The Gamma Knife, which is one of the very first surgical robots, works on the principle that a patient’s skull is fixed in one place—so the device can rotate from that point to fire a beam of radiation to a very accurate location,” he said. “When you are dealing with a rigid, fixed part of the body, algorithms work very well. It’s the same with joint replacements. You can use the bone for reference. But when you are talking about the abdomen, where things aren’t as well defined, it becomes a lot harder.”
Goldberg said we’ve known for some time that AI algorithms can perform at a high level when they are in this kind of constrained environment—but when you want to start considering algorithms that expand across the human body, all that control goes out the window.
“AI is great at playing chess or Go,” he said. “But as soon as you say, ‘Let’s change the rules and hide the things you need to find your way,’ it gets a lot more complicated. How can we design and build systems that can adapt on the fly? That’s what we need to figure out.”
Systems like Goldberg’s Motion2Vec learn their skills by drawing on the expertise of the world’s best surgeons. And, even there, said Krieger, there is incredible variability in how different surgeons accomplish the same tasks.
“The art of surgery comes from the skills that different surgeons have developed over years and years of training,” Krieger said. “There are so many subtle differences in how they do certain things, how they react to different situations—it’s quite complicated. If we look at their behaviors to develop an algorithm for a robot, it’s not so easy to determine what’s the right way to do things. It’s not like using a robot to autonomously assemble an iPhone where a specific screw has to be placed in a certain way.”
Small moves and big differences
When asked what surgeons can do to prepare for this brave new world of surgical intervention, Goldberg said that many of today’s medical students can prepare by playing video games.
“As it turns out, developing the ability to operate a small console in your hand while looking up at a screen; visualizing yourself inside an environment and then navigating that environment effectively is something that can help you to adapt more easily to these kinds of new surgical systems.”
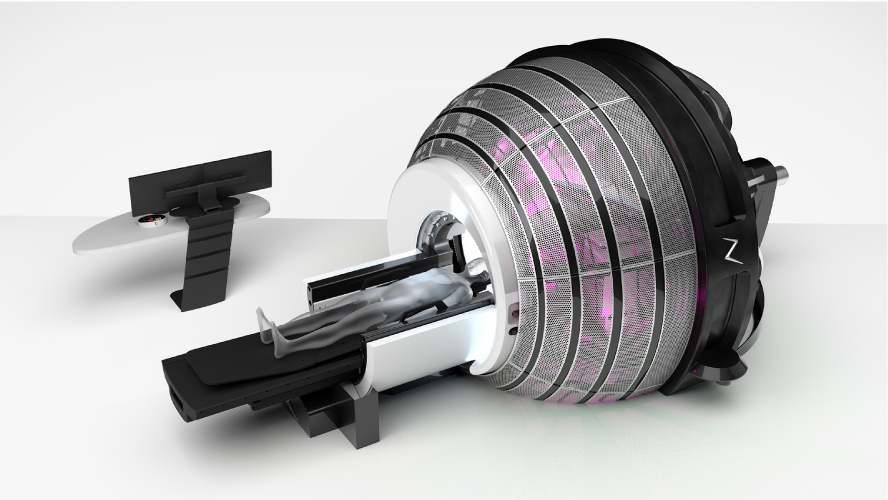 Gyroscopic radiosurgery systems like ZAP-X help neurosurgeons and radiation oncologists to leverage precision radiation. Photo Source: ZAP® Surgical Systems
Gyroscopic radiosurgery systems like ZAP-X help neurosurgeons and radiation oncologists to leverage precision radiation. Photo Source: ZAP® Surgical Systems
Adler says that he has learned, over decades of practice, how to become a better neurosurgeon incrementally. AI advances will be integrated into different medical applications, including surgical robotics, in a similar way, making small moves that result in big differences over time.
“My experience in the OR allowed me to become a much better neurosurgeon through a whole series of little things over time,” he said. “Many of these improvements are often imperceptible—not only to others, but to me, too. AI works in the same way. With big data sets and neural networks, these systems can learn things we never even considered before. AI can pick up all those little nuances of practice and then insert them into what these robots do in the OR. We’re just getting started—but the possibilities, really, are miraculous. We just need to keep working to get there.”